Data-Based Diagnosis
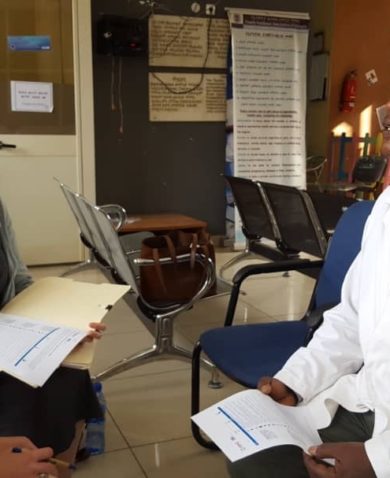
Following a review of baseline assessments and published studies, GHSC-PSM and the Ministry of Health organized four teams to assess 47 hospitals across Ethiopia. The assessment entailed a holistic examination of national health facilities, based on a philosophy of patient-centered design, that focused on easily overlooked details.
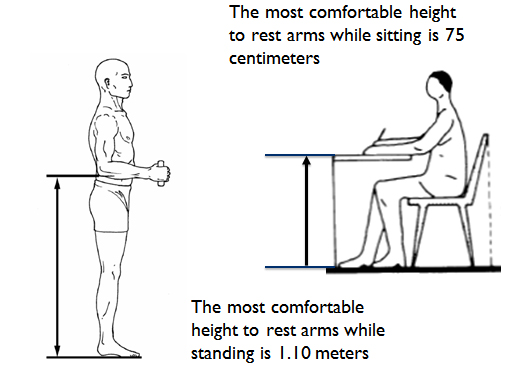
At each of the 47 facilities, the team carefully analyzed and scrutinized every variable — from patient flow to the number of doors and service windows. No stone was left unturned; they even considered the exact height of service counters — down to the centimeter.
The findings showed that patients had to enter three separate queues to get treatment: first to confirm their prescription, then again to pay, and once more to receive medication. Most facilities only had one door, serving as both an entrance and an exit. Facilities also tended to have just one or two service counters, all at varying heights and styles.
These inconsistencies in design were all consistent in outcome: unsatisfactory patient service. Patient flow through three separate queues led to long wait times, poor communication with pharmacists, and confusion about the care they sought. Inconsistent storage capacity led to supply problems. Single doors led to congestion. Insufficient service counters led to inefficient service.
Varying counter heights led to additional issues, including general discomfort as well as difficulties for disadvantaged populations such as mothers, children, elderly, and disabled patients to access the facilities as intended. These issues had affected the staff as well: pharmacists were developing their own medical conditions, such as varicose veins, at facilities with tall counters that required long periods of standing.