Nigeria’s Drug Revolving Fund: A Conversation with Tukur Ibrahim
September 22, 2023 | 5 Minute ReadThe fund helps provide more reliable access to quality medicines and healthcare services at affordable prices, equity in accessing healthcare services, increased patient turnout, and improved patient confidence.
Drug revolving funds (DRFs) are a financing mechanism used in healthcare to improve access to essential drugs and medicines. The primary goal of a DRF is to ensure a steady supply of quality medications and to prevent stockouts or shortages in public health facilities, such as hospitals and health centers.
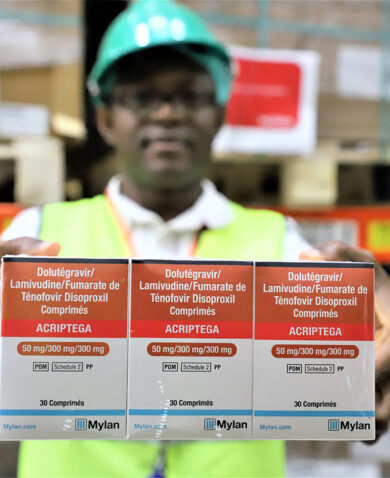
The fund starts with an initial capital injection from the government, international donors, or other sources, which is used to purchase essential medicines and medical supplies in bulk at discounted prices. They are then distributed to public healthcare facilities at affordable prices. The facilities can then sell these medicines to patients at cost-recovery prices plus a small mark-up, often lower than market prices but that covers the medicine costs. Funds from the medications purchased by the patients go back into the revolving fund. This creates a self-sustaining mechanism whereby the money generated from sales is used to replenish and buy more medicines to ensure a continuous supply.
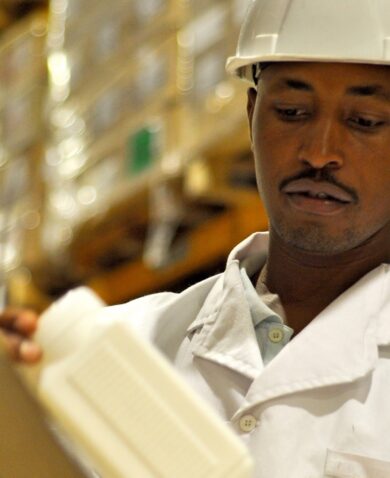
DRFs typically have quality-control mechanisms to ensure that only safe and effective medicines are procured and distributed. This involves proper storage, monitoring expiration dates, and ensuring adherence to standard treatment guidelines.
To learn more about DRF implementation, we spoke with Pharmacist Tukur Ibrahim, Senior DRF Manager in Nigeria for the Chemonics-implemented USAID Global Health Supply Chain Program-Procurement and Supply Management (GHSC-PSM) project.
Could you describe what the DRF is and how it is designed to work in Nigeria?
A DRF scheme uses an initial fund to procure medicines (seed stock) for use in the health system on a user-fee basis for sustainability. Users pay just enough to cover their treatment. The funds collected from users are in turn used to buy DRF products and the process continues.
To ensure the seed stock given is adequate for the DRF, a quantification exercise is conducted and, based on the number of health facilities to be supported, procurement is made to cover them. The type and amount of seed stock to be given depends on the intervention by the donor. Each facility receives seed stock based on patient turnover, warehouse capacity, and availability of human resources for health to manage the commodities.
The DRF strategy ensures adequate protective governance structures are in place before initiating key but vulnerable processes such as investments in seed stock, procurements, distribution, training, and health facility rollout. The strategy is expected to attain a certain minimum level of performance as a prerequisite for health commodity integration at the state level. All the governing structures are to ensure compliance with the DRF operational guidelines and standard operating procedures for sustainability.
Which stakeholders are involved in the execution of the DRF and how is the DRF designed to ensure their continued stability as part of the DRF workflow?
Nigeria’s national DRF guidelines encourage states to establish an agency solely responsible for sourcing, procurement, warehousing, sales, and distribution of drugs and medical consumables for all public health commodities. That is the state Drug Management Agency (DMA), which sources, procures, warehouses, sells, and distributes medical commodities for the DRF. The agency also manages all public health commodities that are not for the DRF. Its running cost is from program sustenance, which is one of the five mark-up elements added to the cost of drugs and medical consumables. The other elements are inflation, monitoring and evaluation, losses and expiries, and deferral and exemption. At the end of every month, the DMA and facilities calculate and disburse the mark-up to the various mark-up elements. The inflation mark-up element is meant to take care of any currency devaluation which will lead to inflation. The accrued money will enable the DMA and facilities to maintain their stock level. Hence, minimal currency devaluation will not have much negative effect on the DRF.
The Hospitals Management Board and State Primary Development Agency own, supervise, and control all secondary and primary health facilities, respectively. The agencies get their running cost from the state, and there are small mark-ups from the services rendered by the facilities that go to the agencies from their respective facilities.
The DRF Steering Committee is a high-level policymaking committee that guides DRF policies and implementation across the state. The Commissioner for Health is the chair, and the Director of Pharmaceutical Services is the secretary. All heads of agencies under the State Ministry of Health are committee members. This committee leverages the mark-up from the services to carry out their roles and responsibilities.
A state DRF committee operates in all states implementing a DRF in Nigeria. It has oversight of DRF implementation at all levels. The membership is drawn from different ministries, agencies, civil society organizations, and community representatives. This committee gets funding from the DRF mark-up to carry out its roles and responsibilities. Each facility that implements the DRF has a DRF committee that ensures the DRF is working at the facility level. The facility DRF committee has funding from the net revenue generated from the services rendered by the facility (internal market operation).
What is the impact on people in the health facilities where the DRF is implemented? Do you have any data that reflects this?
The impact of the DRF includes reliable access to quality medicines and health care services made available at affordable prices, equity in accessing health care services, increased patient turnout at health facilities, and improved patient confidence in accessing public health facilities. Also, because the DRF operates with a small mark-up at public health facilities, it leads to better and affordable prices of medicines and healthcare services in private health facilities because of competition between the two sectors.
For example, the quarterly DRF activities for Muhammadu Abdullahi Wase Teaching Hospital in northern Kano State increased across all parameters. In the first quarter of 2022, 37,055 patients visited the pharmacy, compared to 63,332 in the fourth quarter of that year. Patient turnover at the facility almost doubled from 40,883 to 76,069 in the same period. This indicates increased demand for and availability of quality medicines and healthcare services. An increase in enrollees for the National Health Insurance Scheme and State Health Contributory Scheme also indicates the community has confidence in the facility.
Could you highlight some of the challenges moving ahead for implementing the DRF?
Some challenges include getting strong political buy-in from the state leadership, compliance with the DRF operational guidelines and standard operating procedures, and consistent implementation of the DRF.
Additional challenges include the need for robust monitoring and supervision (M&E) despite a well-structured M&E framework, inadequate funding for stock replenishment, and limited items supplied as seed stock by USAID through GHSC-PSM. For example, USAID provides 22 line items of seed stock for malaria and maternal, newborn, and child health medicines, while an ideal DRF system has more than 500 line items. This means facilities lack a wide variety of DRF commodities. Therefore, the DMA has to use the sales from the 22 line items of seed stock provided to procure other line items to satisfy the total stock needs at the facilities, contributing to stockouts of the DRF items.
Another challenge to the DRF is ensuring cash and carry to minimize the risk of de-capitalizing, which is when a DRF facility loses from its initial fund value provided as capital. It is one of the important guiding principles of the DRF. It stipulates that the payment for DRF items should be collected at the time of delivery at all levels: between DMA and health facilities, between health facilities and their respective service units (Internal Market Operations), and when dispensing DRF items to patients.