Going to a health care facility to pick up antiretrovirals (ARVs) became a precarious task for the approximately 38 million people across the globe living with HIV during COVID-19. The risk of exposure while accessing essential services and counseling suddenly became too high for immunocompromised patients. As the situation unfolded, the global health community grappled with a difficult dilemma —protecting health workers and patients from exposure while ensuring continuity of services for people living with HIV (PLHIV).
Ensuring continuous access to treatment and services is critical to staying on track to achieve UNAIDS 95-95-95 goals by 2030. To fast-track the progress made, 95 percent of PLHIV who know their status need to be on ARV treatment. The global health community, including the USAID Global Health and Supply Chain Program–Procurement and Supply Management (GHSC-PSM) project, is acting quickly to make sure that this progress is not lost to the global disruptions that the pandemic has generated. One key solution is protecting health workers and immunocompromised patients with differentiated service delivery. This delivery method focuses on clients to simplify and adapt HIV services to serve PLHIV while reducing unnecessary burdens on the health system.
Epidemics don’t stop being lethal during pandemics
Adapting to COVID-19 has been a major challenge for PLHIV, who require continuous access to therapy and services to stay healthy. Before COVID-19, it was already challenging for many people in rural areas to access care at the nearest health center because of poor road infrastructure, overburdened health posts, internal conflict, natural disasters, and the lack of last-mile services. In Namibia where HIV/AIDS is the leading cause of death, and more than 200,000 PLHIV need constant access to medication, 84 percent of the country roads are unpaved, making it difficult to reach the closest pharmacy or health center even before COVID-19. Continuity of services during the pandemic is critical, which is why the U.S. President’s Emergency Plan for AIDS Relief has focused on expanding multimonth dispensing (MMD) of ARV to PLHIV.
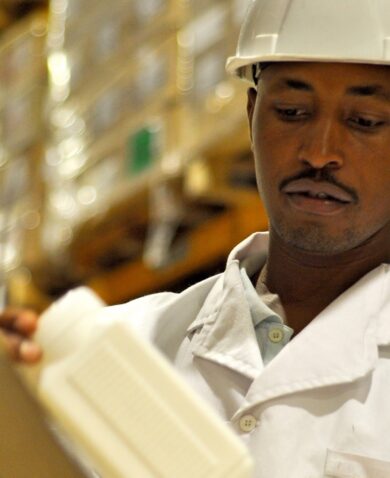
MMD reduces the PLHIV risk of exposure by providing an increased supply of drugs, from 30-tablet bottles to 90- or 180-count bottles. So, instead of picking up a monthly supply, PLHIV can obtain a three-to six-month supply, decreasing their travel. Fewer trips to the pharmacy also means decongestion at the health facility and less exposure for patients and health care providers, ensuring social distancing and preventing COVID-19. By the end of 2020, GHSC-PSM had delivered 13.9 million 90-count bottles and more than 200,000 180-count bottles of tenofovir, lamivudine, and dolutegravir (TLD) to 20 countries over the life of the project.