Recommendations for a Diverse, Sustained Health Workforce
February 27, 2020 | 4 Minute ReadHow do we establish higher-performing health systems to achieve universal health coverage? These three key recommendations focus on building a diverse workforce to deliver accountable, affordable, accessible, and reliable health care for all.
There are simply not enough health workers to meet the basic health needs of all people worldwide.
This prevents development practitioners from contributing to higher-performing health systems, as we struggle to make the most with the health professionals we have available, who are often concentrated in urban areas, working in professional silos, and failing to reach the most underserved populations. Additionally, health system leaders struggle to adequately manage the current health workforce and plan for the future by failing to support health workers’ professional growth and ability to deliver high-quality services efficiently.
By transforming the global health workforce, we can transform health systems to deliver for all. But don’t just hear it from me, hear it from Dr. Lazare Coulibaly, USAID Human Resources for Health in 2030 (HRH2030) Program Deputy Director in Mali. Lazare and I, along with two of our other colleagues in the global health community—seen here via video clips—all spoke about the need for a diverse, sustained health workforce at the recent Prince Mahidol Award Conference, Accelerating Progress Towards UHC.
Continuous, cost-effective, and integrated primary health care requires a more diverse mix of skills and types of health workers to support countries’ journey to self-reliance. Here are some opportunities to diversify and sustain the health workforce.
1. Harness the role of performance management and community-based workers to optimize health service accessibility.
In Mali, many remote health workers have not been visited by a supervisor since 2012 due to security concerns and limited resources. The HRH2030 Program in Mali is using optimization tools like innovative supervision and mentoring approaches to promote higher-performing health care services at even the most remote facilities. By digitizing national supervision checklists and empowering health workers with a tablet, they can conduct self-assessments so district supervisors can understand their performance levels and provide remote coaching and support. These data are more easily shared and integrated with service delivery information to understand and strategically address gaps, which makes health care services more reliable, motivates health workers to stay at their jobs, and sustains communities’ access to care. Watch Living Goods Deputy Country Director Ruth Ngechu explain the community-based approach in Kenya.
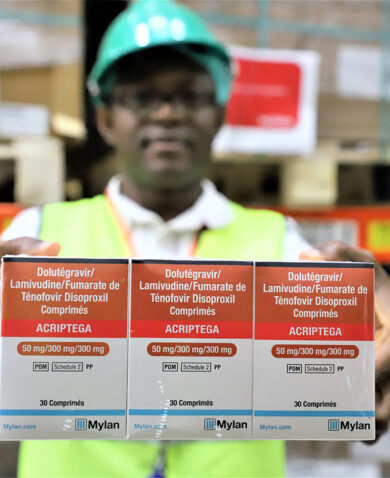
Better performance management is important to support all frontline health workers. The WHO’s community health workers (CHW) guidelines recognized CHWs as essential contributors to primary health care. As such, they need to be connected to the rest of the health system. For example, as CHW and an HIV-positive mother herself, Margaret Odera improves access to prevention of mother-to-child transmission (PMTCT) services through referrals to care in the Nairobi slums. Margaret has been very effective, in part because she is from the community, is trusted, and understands families’ challenges accessing health care.
2. Improve the interoperability of information systems to manage and plan for a health workforce that understands current and future needs.
All health policymakers want to know—and are perennially challenged to answer—what seem like simple questions: How many health workers do we have? Where are they? What are their skills? How are they performing?
While the WHO’s National Health Workforce Accounts provides a common structure for country stakeholders to progressively report to, investments in national human resources for health information systems present an opportunity to better understand the answers to these questions. It’s essential to have reliable, up-to-date, complete, and high-quality health workforce data for planning and decision-making at the country level. According to the HRIS Status Review completed in Indonesia by HRH2030 last year, there are more than 10 government agencies — including health, education, labor, public service, and other sectors — that collect data on health workers. Integrating this data, including economic, epidemiological, and demographic trends, could facilitate building a more complete picture of health workforce priorities in a country.
HRH2030 in Indonesia is also supporting the Ministry of Health to overlay interoperable data to quickly and comprehensively inform policy solutions. For example, data visualizations that illustrate the location of people with high blood pressure overlaid with health workers’ locations, or the locations of newly graduated nurses, can enable health system stakeholders to make smarter decisions about which health workers to train and where to prioritize resources.
3. Diversify health professionals to build more career pathways for women and under-represented youth.
Globally, health care is delivered by women and led by men. Women represent 70 percent of the global workforce, and only 25 percent of senior leadership roles. Indeed, women, youth and community-based health workers are key to improving health equity by representing the patients they serve and reaching the hardest to reach but their roles are under-recognized.
There is a disconnect between the 71 million unemployed youth worldwide and the estimated 40 million new health jobs that need to be created by 2030, which means that we need to look critically at how we prepare career pathways in community-based health. HRH2030’s framework identifies opportunities for technical, vocational, and educational training institutions to better support under-represented youth to succeed by addressing the cultural and socioeconomic barriers to enroll and complete health studies and collaborate with the health sector to produce graduates that respond to population health needs. Employers also need to rethink their support to these more diverse employees and their work requirements, including adequate family leave and protection from sexual harassment and discrimination, to ensure health workers stay.
As 2020 is the International Year of the Nurse and the Midwife, let’s apply these recommendations and invest in higher-performing health systems for nurses and midwives, who make up about half of the global health workforce. The impact of this investment could be exponential, as many nurses manage both primary health care facilities and community health workers, often with little to no support. The Nursing Now campaign has formed local chapters in more than 100 countries to elevate nursing leadership. With empowered nurse and midwife leaders today, the future workforce can be lifted by their example.
Health workers strive daily to save lives and keep people healthy, let us support them. USAID’s HRH2030 Program has announced its Health Workforce Resilience Prize. Please share, nominate someone, or apply!
*Banner image caption: Patient and doctor during a consultation in Indonesia. Photo credit: Chemonics/Andi Gultom
Posts on the blog represent the views of the authors and do not necessarily represent the views of Chemonics.