Information is Power
Any efficient supply chain needs a well-designed information system. Without that, the alternative is usually manual data collection and hand calculations, resulting in a supply chain that is untimely, inefficient, and unreliable. Accessing that quick and reliable data is the difference between health clinics with accurately stocked shelves and those that are hundreds of treatments short due to one miscalculation. With an electronic logistics management information system (LMIS) at their disposal, health facilities have a system that aggregates, analyzes, and validates data on the availability of medical commodities.
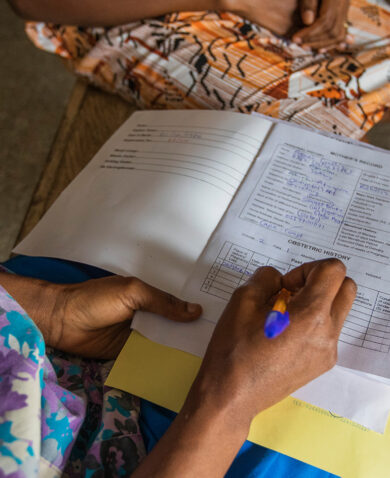
Nuran Adris Mallya is an OpenLMIS specialist for the USAID Global Health Supply Chain Program-Procurement and Supply Management (GHSC-PSM) project. “Imagine a country that has thousands of health facilities and all of that information is being collected on paper,” she explained. “It’s very difficult to manually aggregate all of that data to inform decision-making. For example, if there is a stockout in a facility, it’s important to know as soon as possible. OpenLMIS automates this process.”
With support from the GHSC-PSM project, Malawi’s health supply chain is experiencing this transformation first-hand.

A New Tool, A New Level of Transparency
In Malawi, more than 600 health facilities are tasked with reporting the medical commodity stock on hand, rates of consumption, and how much more medicine is needed. For 13 years, these facilities collected information with a system that generally produced the right data, but couldn’t deliver it to the right place, at the right time, and for the right cost.
What makes OpenLMIS different? One major advantage is that OpenLMIS is web-based. For health workers across the country, this eliminates the need to install a new system on their computer and manually submit their LMIS data via email. Even when internet connectivity is limited, they can still work offline. OpenLMIS also aggregates real-time data from across the country into a single, cloud-based database. For Malawi’s Ministry of Health, this eliminates the need to travel to dozens of districts and central hospitals to back up each site’s individual database.
GHSC-PSM, in partnership with VillageReach and Malawi’s Ministry of Health, launched OpenLMIS in August 2017. The new system not only expedites data entry, but also brings visibility to processes that were once a blur.
“OpenLMIS encourages facilities to request stock based on their consumption,” said Nuran Adris Mallya. “If your consumption is 50 packs of a commodity per month, you should probably order 100 packs of a commodity, and not 1,000. The new system flags this and anyone who has access to the system can see a discrepancy.”
For district pharmacy technicians in Malawi who submit monthly reports, this technology makes an enormous difference.
“The fact that OpenLMIS is balancing my records increases my confidence in the data generated by the system and also provides a starting point to inform supervisory visits to facilities in my district,” said a pharmacy technician in Blantyre, Malawi.

Technology is a Means, Not an End
As with any transition to new technology, the OpenLMIS pilot in Malawi encountered challenges. Facilities in Thyolo, Lilongwe, and Mangochi faced power blackouts and connectivity issues that contributed to the lack of reporting from the new system. In Machinga, reporting rates dropped due to staff absence during the December 2017 holiday season.
However, buy-in at the central and district levels made it possible for teams to learn a new system, embrace its potential, and realize the true impact of data being shared along the whole supply chain. During February 2018, the reporting rate was 95 percent for the essential medicines program, 93 percent for HIV, 94 percent for malaria, 92 percent for reproductive health, and 93 percent for tuberculosis. The system now operates in 33 hospitals and five health facility hubs across Malawi.
As GHSC-PSM continues piloting OpenLMIS in other countries, the technology must adapt to new challenges and dynamics. Some countries might be transitioning from paper-based reporting. Other countries might face resistance to the level of oversight that OpenLMIS stimulates. In any context, adequate training and a culture of transparency are key. When the end goal is saving lives through the reliable availability of medicines and treatments, technology like OpenLMIS takes us one step closer to making this a reality.