Communities Together —Accelerating Uptake of Promising New HIV/AIDS Medicines
December 6, 2019 | < 1 Minute ReadWith potential new HIV treatment options on the horizon, how can a successful transition between regimens be secured at a country and local level? Drawing on our USAID Global Health Supply Chain Program-Procurement and Supply Management (GHSC-PSM) project’s recent role in the transition to TLD – the currently preferred first-line ARV – we share some advice.
This post originally appeared on Devex.
While the global HIV/AIDS community has made great strides toward the Joint United Nations Programme on HIV/AIDS’ 90-90-90 goals and the U.S. President’s Emergency Plan for AIDS Relief’s epidemic control goals, there is still a long journey ahead to end the AIDS epidemic by 2030.
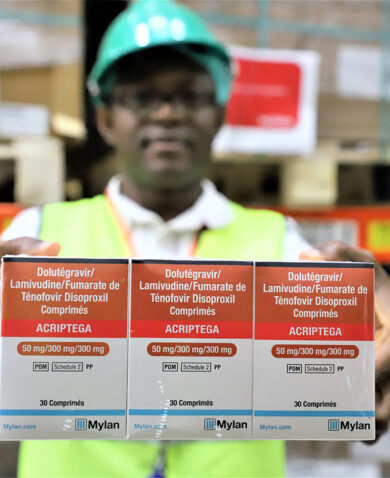
Critical to the global HIV/AIDS community’s efforts is ensuring people living with HIV have access to the latest antiretroviral drugs that effectively suppress viral load. Suppressing viral load can help people live longer and healthier lives, prevent mortality and opportunistic infections like tuberculosis, and minimize transmission of HIV to uninfected partners or during pregnancy.
“We need to get better — and faster — at bringing new treatment regimens to the patients who need them,” said Nagesh Borse, acting director for the HIV/AIDS task order on GHSC-PSM.
Fortunately, clinical advancements have given rise to new, more effective medicines with less severe side effects. However, once a new medicine is tentatively approved by a drug regulatory agency — the U.S. Food and Drug Administration, for example — bringing it to market at a global scale is highly complex, particularly in low- and middle-income countries.
In the U.S. it takes approximately five years to transition to a new drug. In Africa, it can take 10 to 20 years to get more than 80 percent of the population onto a new medication. We need to get better — and faster — at bringing new treatment regimens to the patients who need them… Read the full article on Devex.
Posts on the blog represent the views of the authors and do not necessarily represent the views of Chemonics.