20 Years of Evolution in Human Resources for Health
May 23, 2016 | 3 Minute ReadThe 69th World Health Assembly presents a significant milestone for those of us who work in human resources for health (HRH): HRH has finally been recognized as a foundational principle in reaching world health goals. More so now than at any other point in history, the public health community is devoting significant attention and effort to making sure that the right health worker is in the right place, with the right skills and motivation, to provide high-quality service in order to reach universal health coverage.
This year, the World Health Assembly will formally adopt the WHO Workforce 2030 strategy, and designate the National Health Workforce Accounts as the basic data set for HRH informatics worldwide. The WHO Health Data Collaborative is creating an HRH working group, and fit-for-purpose HRH was recently recognized as a necessary condition to reach the Sustainable Development Goals (SDG 3).
With HRH in the spotlight, it’s easy to forget that as recently as the mid-1990s, the public health community had only a rudimentary understanding of how to strengthen the health workforce. At that time, paying attention to HRH meant little more than training health care providers. In these last 13 years, though, we have seen elemental changes in the sophistication and effectiveness of our HRH research and interventions.
This transformation began in the late 1990s with the realization that even the best training alone wasn’t enough to help providers deliver the best care. The health community began promoting performance improvement approaches to ensure an enabling environment for health care workers, yet the focus was still on improving the individual provider.
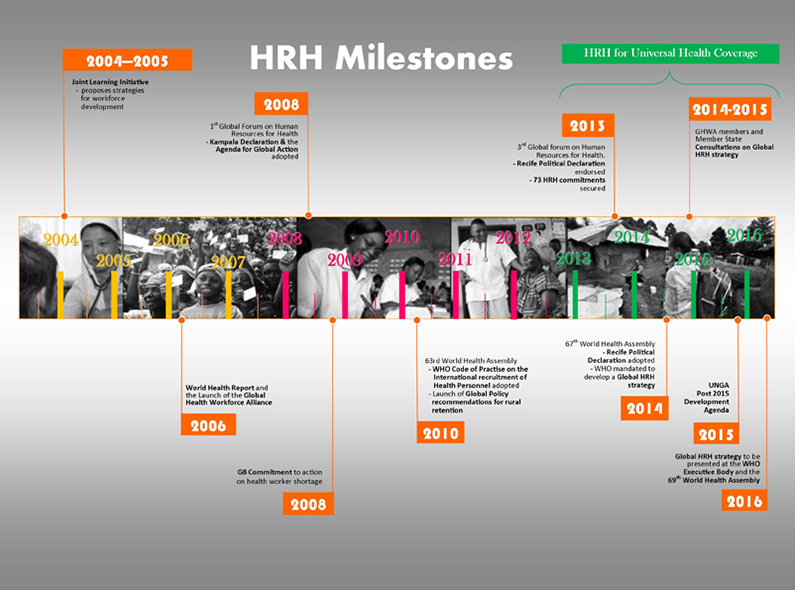
Human resources for health milestones since 2004, according to the World Health Organization.
In the early 2000s a visionary group from WHO called the Joint Learning Initiative (JLI) began to collect data and look for research on the health workforce writ large. The group, led by Dr. Lincoln Chen, began conducting landscape analyses of the number of providers as compared to the population, and examining the effect of this ratio on health outcomes. In 2003 the JLI published their seminal report Human Resources for Health—Overcoming the Crisis, launching the idea of HRH as a linchpin of the health system. With it came the provider/population ratios that we still use today: in order to reach the Millennium Development Goals (the predecessor to the SDGs), a country needs at least 2.8 health care providers per 1000 people.
Compared to the National Health Workforce Accounts’ 250 indicators and the plethora of elegant research analyses now being conducted on HRH, the 2.8 ratio seems today a blunt instrument. But in 2003 the JLI report served as a wake-up call and the start of the light-speed progress that brings us to WHA 2016.
In the intervening years, a subsequent World Health Assembly focused specifically on the health workforce and how it could be measured, strengthened, and sustained. In 2004, USAID launched the first global flagship project focused explicitly on HRH, the Capacity Project. During the same timeframe WHO launched the Global Health Workforce Alliance, a partnership of more than 400 organizations coming together to find common solutions for HRH problems.
Over the past two decades, we have moved beyond simple but necessary questions such as how to improve retention, and are now seeking ways to optimize the health workforce that is already in place. Simple provider/population ratios have given way to analyses that include forecasts of disease burden, provider competencies, geographic distribution, and migration trends. The world of health informatics has changed the quest for human resource information from one of moving from paper files to simple databases, to building interoperability among existing government systems such as Civil Service databases, DHIS-2 health databases, automated payroll systems, and social security insurance data. While good training and performance improvement efforts will always be necessary, a focus on optimization has revealed the need to help existing providers be as productive as they can be. Likewise simple incentives and pay-for-performance schemes are being coupled with research and interventions on how to maximize the intrinsic motivation providers already feel in serving their fellow community members.
For those of us who have been on this HRH bullet train from the mid-90s to the mid-2010s, it may be tempting to pause for a moment and take satisfaction in how far we’ve come. But let’s only allow ourselves a moment, before digging in for what we hope will be even more accelerated progress in the next two decades.