When There Is No Money to Hire More: Helping HIV/AIDS Health Care Workers to Be as Productive as They Can Be
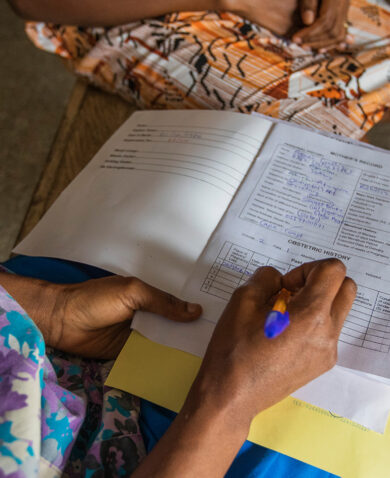
December 1, 2015 | 2 Minute ReadA health care worker tests a woman for HIV in the Democratic Republic of the Congo.
We need to face facts: In many developing countries, there simply isn’t any money to hire more health care workers. According to WHO there is a global shortage of more than 7 million health care workers; 83 countries fall below WHO’s basic recommendation on of 23 health care providers per 10,000 population. By 2035, that shortage is expected to grow to almost 13 million.
The situation is even worse for HIV/AIDS care providers. According to research conducted by the President’s Emergency Plan for AIDS Relief (PEPFAR), in many countries HIV/AIDS provider vacancy rate is between 50 and 75 percent. Exacerbating the problem, existing HIV/AIDS providers do not have what they need to be as productive and perform as well as possible. While rigorous studies of health care worker productivity in developing countries are relatively rare, a 2011 USAID Health Systems 2020 study in Zambia found that nurses spend only half their time in productive patient care, 22 percent on other work tasks such as paperwork, and the rest of their work day in non-productive activities.
And yet studies in Malawi and Uganda have shown that providers have a high level of intrinsic motivation to serve their communities and give high-quality care. They are often held back by simple, locally solvable problems such as lack of basic inexpensive supplies, supportive supervisors, or freedom to shift tasks to colleagues with ample time (e.g., assign paperwork to trained clerks). In rural Ethiopia, I saw dedicated, hardworking HIV/AIDS providers thwarted in their desire to provide high-quality care to their fellow villagers by a lack of supplies that they could, but were not allowed to, buy in the local market.
In response to this opportunity to get more and better service delivery from the existing workforce, the U.S. government, through USAID and PEPFAR, has made clear plans to address the issue. PEPFAR recently released its Human Resources for Health (HRH) Strategy. Objective 5 of the strategy’s five-objective agenda is “Improve health worker performance at moderate- and high-volume sites and/or high HIV-burden areas for service quality.” USAID recently renewed its commitment to addressing the HRH issue by partnering with Chemonics to manage a five-year project designed to help developing countries cultivate the workforce needed to reach sustainable health development goals, including achieving and maintaining an AIDS-free generation. The project, Human Resources for Health 2030 (HRH2030), has as its first objective to support primary providers to be as productive as possible and to perform up to standards of high-quality care.
Even early in project startup activities, HRH2030 has plans to increase the productivity of PEPFAR-supported HIV/AIDS providers in at least two countries and to develop a supportive environment for improved provider performance to deliver high-quality HIV/AIDS care. According to James Griffin, the HRH2030 project director, “There has been a significant amount of funding put into supporting an array of HIV/AIDS service providers. What is important now is to ensure that human resources at service delivery sites are reaching their maximum potential.”
HRH2030 aims to ensure that every provider has what they need to deliver the high-quality care they are already motivated to deliver.