3 Questions with Mary Lyn Field-Nguer: Transitions in How We Prevent and Treat HIV
December 1, 2016 | 3 Minute ReadIn honor of World AIDS Day, Mary Lyn Field-Nguer reflects on the evolution of HIV prevention and discusses big transitions in treatment.
1. What supply chain challenges inhibit universal access to HIV/AIDS prevention, treatment and care?
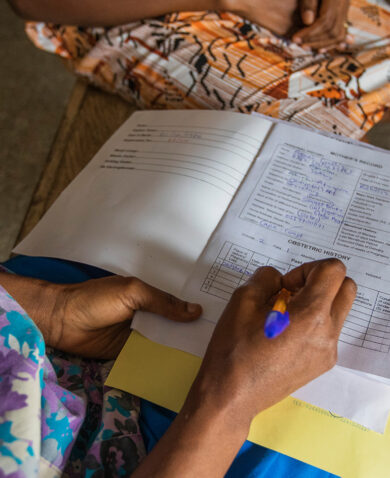
The treatment of people with HIV presents unique challenges. Even once people are on treatment, they must be monitored to be sure the drugs are effective in decreasing the person’s viral load. WHO guidelines supported under the President’s Emergency Plan for AIDS Relief (PEPFAR) calls for countries to adopt testing antiretroviral therapy (ART) patients’ viral load rather than monitoring their CD4 counts. Making it possible for people to access viral load testing on a wide scale requires a lot of work on the part of governments and donors. Countries are undergoing a transition that requires a lot of supply chain support in terms of procuring reagents, strategically placing of viral load instruments around a country, and decommissioning CD4 machines, all requiring close coordination between government, donors and implementing partners.
Scaling up viral load testing is part of the 90-90-90 targets — the third target means that, by 2020, 90 percent of people with HIV will have a suppressed viral load. In addition, there must be enough rapid test kits in a country so that the first 90 is met — that 90 percent of people with HIV know their status. The second 90, that 90 percent of people with HIV have access to treatment, requires a functional supply chain from beginning to end. The correct number of antiretrovirals (ARVs) must be ordered and delivered to the country in time to meet the needs of clinical sites, so that sites have enough drugs to treat patients with no stock outs.
2. As the global health community rallies around the 90-90-90 targets to help end the AIDS epidemic, what successes or innovations can we draw upon?
Right now, we’re focused on providing guidance to countries on implementing multi-month dispensing, which involves providing or dispensing to patients three to six months of ARVs at a time rather than the traditional one month supply. This approach will help decongest clinics and decrease the travel demands on patients. Overall, it has the potential to decrease the costs of delivering treatment in a country. GHSC-PSM is providing technical support to countries for whom this is new so that the necessary supply chain adaptations occur to ensure a smooth transition.
We are also working to better integrate supply chains at the country level so that parallel supply chains aren’t operating for different diseases. Under an integrated system, for example, a delivery truck might provide a clinic with commodities for both malaria and HIV in the same trip, making the system more efficient.
In terms of innovation, there will be a day soon when unmanned aerial vehicles (UAVs) or drones will be seen transporting drugs, blood samples, or bags of blood for transfusions to clinical sites in Africa. This is an innovation that GHSC-PSM will be prepared to support.
3. How have approaches to HIV treatment and prevention evolved in the post-2015 development agenda?
I touched on this in my previous blog post about achieving the 90-90-90 targets. When I started working in this field, there was no HIV testing available in countries in Africa. I was the managing editor for the first training manual for clinicians in sub-Saharan Africa that covered the management of opportunistic infections. Soon after publication, PEPFAR was born, and ARV access in those countries followed soon thereafter. One section of the training manual covered ARVs, and it became the most important part of the manual — something that we would not have been able to predict in 2000.
It is amazing that countries will now treat people as soon as they test positive for HIV rather than waiting until their CD4 count is low and they are suffering from opportunistic infections. GHSC-PSM is on the alert to meet this increased demand for ARVs. This theory, that we can stop HIV transmission if we can get enough people on treatment in a country to reach a tipping point, is a huge change. Reaching that tipping point would mean the end of AIDS — something we all dream of and are working tirelessly to make a reality.