3 Questions with Grace Namaganda: Balancing Service Delivery for HIV/AIDS, Malaria during COVID-19
September 1, 2020 | 4 Minute ReadGrace Namaganda, the country director of the USAID Human Resources for Health in 2030 (HRH2030) program in Malawi, explains how her team is working to protect immunocompromised patients and community health workers in the face of COVID-19.

The fight to end HIV/AIDS is far from over, and millions worldwide rely on services or commodities that aren’t designed to work with social distancing rules. Grace Namaganda provides recommendations on how to use data for decision-making, protect community health workers, help HIV patients adhere to antiretroviral (ARV) regimes, and leverage partnerships from her experience in Malawi.
1. What are some examples of using data for informed decision-making as we continue to fight epidemics, like HIV and malaria, in the face of a pandemic?
The COVID-19 pandemic has highlighted the need for accurate, accessible, and timely data. In epidemics and pandemics, you need to keep monitoring the situation because it keeps changing. For the HIV epidemic, we monitor the situation every quarter with PEPFAR’s support, ensuring that we are collecting accurate data to respond appropriately. And for the COVID-19 response, the Ministry of Health established a task force to gather advice from a variety health partners. We meet every week to share data, and we have seen the data needs changing over time as decisions that need to be made also change.
In Malawi, the pandemic started slowly; we did not have a lot of cases and deaths. Initially, we needed data for assessing the situation and addressing gaps. Later, we focused on planning for returning citizens and residents, so the data needs changed because we needed to figure out how to keep these people safe and well cared for. But now, we are in the middle of the COVID-19 pandemic, and the number of cases and deaths keeps rising. Now we need real-time data to track cases and assess testing and treatment capacity, to enable us to make constant improvements to our response. Ensuring data-driven decision-making is particularly important now because in Malawi, like in many other countries, the increase in COVID-19 cases is putting a strain on the limited resources for provision of health services. The task force can’t discuss COVID-19 alone because care for other diseases also must continue. Health service delivery is not done in isolation, and we need to maintain services for malaria and HIV/AIDS as well to avoid losing the progress we have made to fight these diseases.
2. With the success rates of community-based models compared to facility-based models, what can we do to keep community health workers safe while they help HIV patients adhere to their regimes?
There are two different levels of service for community-based models: the individual level, where services target an individual client, and then there are also services that target a group of clients, through which HIV positive patients come together, share lessons, counsel each other, and receive different services such as counseling and ARV refills. In both cases, the community health worker interacts with the community and therefore is at risk of contracting COVID-19. So, to start with, the global health community must make sure that we are protecting the community health workers and ensuring their safety. In the Malawi context, the first thing the task force did was train them on how to protect themselves against COVID-19. And then, we made sure they had personal protective equipment (PPE) and that facilities were sanitized. Unfortunately, some services such as community mobilization, testing, and tracing still need to be created, and the lack of available PPE to ensure the safety of community health workers is curtailing active defaulter tracing.
As a policy in Malawi, community health workers are provided with personal protection supplies such as hand sanitizer, face masks, and shields to minimize contact with clients while offering services. As we continue to plan for the response, I think that one of the improvements to keep community health workers safe is increasing their numbers to reduce their workload. If people are overworked and burned out, there is a greater chance for errors that could potentially expose them to COVID-19. To address this, the government of Malawi recruited 2,000 health workers to support the pandemic response. The other improvement I would suggest is to take precautionary measures to minimize transmission when community health workers meet with an individual or a group, such as ensuring social distancing and having fewer participants in community group sessions. Another way to protect community health workers is reducing the number of times they meet immunocompromised patients by switching to multi-month dispensing models.
One more option is to explore the use of technology, particularly telephones. Adherence counseling and reminding people to go to facilities for treatment can all be done over the phone, reducing face-to-face interaction thereby avoiding unnecessary exposure. Community health workers can also be provided with individual transportation means like bicycles and motorcycles to minimize the possibility of getting infected from using public transportation. Lastly, protecting the community is also key because if members of the community are healthy, they will not expose the community health workers.
3. How can integrated partnerships and multisector alliances continue to support community-based programming to combat HIV?
Partnerships are important because of the wide scope and costs involved in designing and providing community-based programs for HIV/AIDS. The community service needs are many, starting with prevention, care, and treatment and moving to viral suppression. The resource needs are also many, so governments and implementing partners need to collaborate with other stakeholders to provide health workers not only fair salaries and allowances, but also with the resources they need to serve the communities better.
There are several partners working at the community level in Malawi, and one of the major challenges is not lack of resources but lack of coordination. Ensuring synergy between partnerships is critical in all aspects of the response. For example, as global health practitioners advocate for multi-month dispensing, we need to think comprehensively about all the resources we need, such as medicines which sometimes may not be adequate. Here is where partnerships can be useful. For example, if one partner is good with supply chain management, they can handle that part; and if another one is good at human resources for health, they can handle that. The components of community-based programming are many, and they would benefit from different expertise but also from collective resources to ensure cost-effectiveness and to provide quality services to communities. I urge partners and donors to work collaboratively with the governments they serve to ensure coordination and together we will achieve more in combating the HIV/AIDS epidemic.
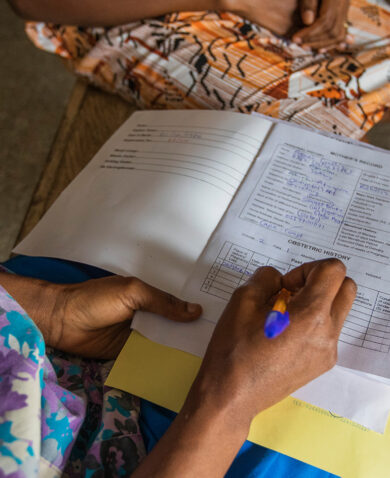
*Banner photo caption: Community health workers in Malawi. Photo credit: HRH2030 Program Malawi.
Posts on the blog represent the views of the authors and do not necessarily represent the views of Chemonics.