3 Questions with Baz Semo: Ensuring Safe and Continuous HIV Service Delivery in Nigeria
December 14, 2020 | 4 Minute ReadCOVID-19 is threatening to reverse progress toward epidemic control in Nigeria. Find out how we are helping healthcare providers and communities change how they deliver services critical to controlling the nation’s HIV epidemic in the face of the pandemic.

In Nigeria, where 1.8 million people live with HIV and 100,000 were newly infected in 2019, the pandemic has disrupted the government of Nigeria’s efforts to lead a large-scale, evidence-driven national response to control the HIV epidemic by limiting access to critical testing and treatment services. To address this, healthcare administrators and frontline workers are examining new ways to safely reach people and offer HIV services by shifting service delivery and care from facilities to communities; leveraging existing, low-cost digital solutions and technologies; and scaling up multi-month dispensing (MMD) and other differentiated service delivery strategies that reduce exposure. Global Health Division Managing Director Baz Semo explains how the USAID Nigeria Strategic HIV/AIDS and Tuberculosis (TB) Response Program (SHARP) projects are working with healthcare facilities and communities to adapt HIV service delivery and ensure safe and continuous access to care and services.
1. How have the SHARP projects, Task Order 1 (TO1) and Task Order 3 (TO3), worked to support continuous access to health services during COVID-19? Are there any health areas that have been particularly affected?
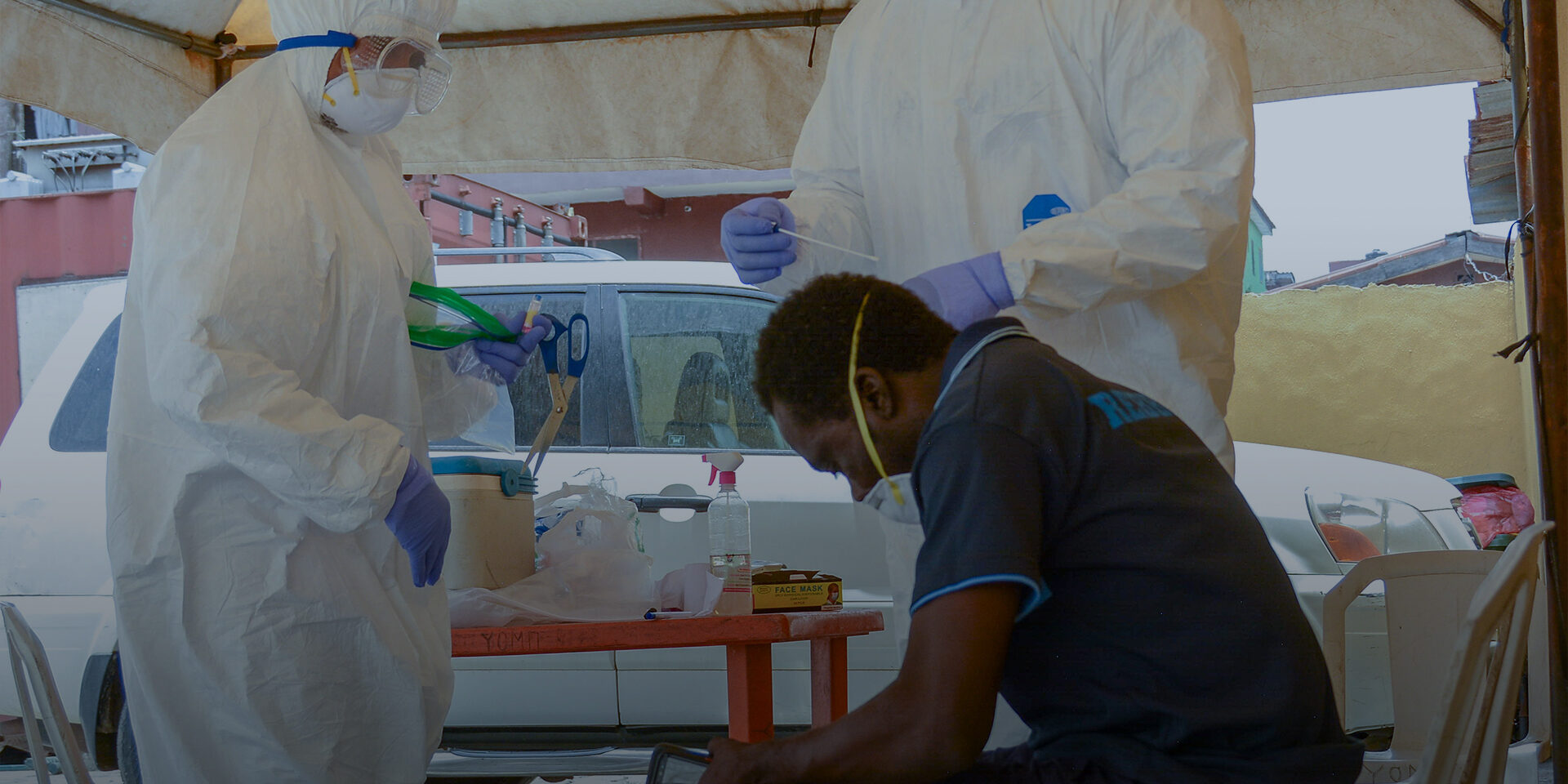
At the start of the pandemic, lockdowns and movement restrictions as well as the population’s fear of contracting COVID-19 impacted delivery of HIV services in all the states, including those in Northeast and Northwest Nigeria. Testing was particularly impacted when people stopped going to health facilities during the onset of the pandemic. We found that between the first and second quarters of 2020, the facilities we support in Northwest Nigeria were diagnosing 15 percent fewer people with HIV. To address the gap in HIV case finding, the projects used geo-mapping and facility-based historical data to identify people living with HIV in the community and select targeted hotspot testing sites.
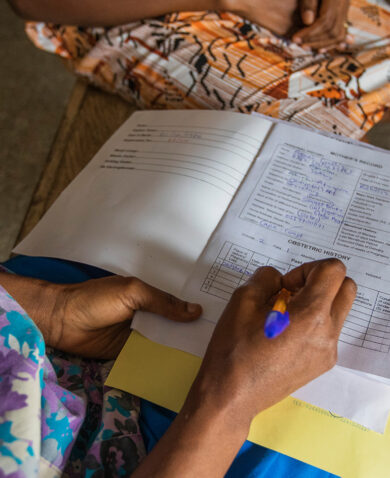
A lot of existing patients were also missing regular follow-up appointments to get their medications or get a viral load (VL) test because of the pandemic. We needed to respond to the declining number of patients seeking services and protect investments made towards epidemic control, so our project teams immediately started examining and designing approaches to move services closer to the patients. Most notably, this included assembling community teams consisting of trained counselors, testers, expert clients, and laboratory technicians – using personal protective equipment (PPE) – to provide safe HIV case finding, antiretroviral (ARV) refills, and VL sample collection in the community.
In addition to this, we worked with facilities to help establish a staggered clinic appointment system for patients who absolutely needed to visit facilities for treatment and established more pickup points in the community, including patient-led ARV refill groups, community pharmacies, and identified private vendors who could dispense medication in the community. The teams also scaled up MMD to over 90 percent of patients and even to new patients who appeared willing and ready to adhere to ARV treatment.
The SHARP projects had begun prioritizing community ARV refills and VL sample collections from the beginning of the projects. What is really fascinating is that after scaling these interventions due to COVID-19, we saw significant improvements in results in the months following the lockdowns and movement restrictions. For example in Northwest Nigeria, the project teams were able to test almost three times the number of clients and identify close to two and a half times the number of HIV positive patients from July to end of September 2020 compared to the numbers prior to the lockdowns. Similarly, HIV case finding doubled and retention levels went from 88 percent to 96 percent due to aggressive ‘back to care’ campaigns performed by community teams with support from SHARP TO1 and TO3, local governments, and community health workers.
2. The northwest and northeast regions of Nigeria have experienced continual fragility and security concerns. How has the COVID-19 pandemic impacted the security situation in these regions?
Several strategies were put in place to ensure the safety of project staff, health workers, and patients. There were four strategies that were particularly instrumental:
- SHARP staff assessed the security level of the facilities and the communities they support daily before having staff go out and provide services. They did this by liaising with the Chemonics security team who contacted local sources to gather relevant security information.
- Through a security reporting collaboration with other stakeholders in the states where the projects operate, our teams were able to get regular security reports that helped determine movement.
- Redistributing staff so that they can support the sites closest to their communities of residence which they are more familiar with in terms of security proved to be an effective strategy in mitigating risk.
- Project staff used virtual platforms to counsel patients and provide critical services in an effort to reduce the movement of patients. This was particularly useful among clients with smartphones, data, and digital literacy.
3. What are the key concerns/gaps these projects and local actors face as the pandemic persists? What are some of the key lessons learned from this experience?
In terms of key gaps, the lack of in person engagement with patients hampers the ability of the staff to improve treatment literacy where needed and to identify possible complications or co-infections. This is especially an issue with patients who don’t necessarily have the digital resources or literacy to engage. In terms of unintended consequences, confidentiality of patients’ information became a potential concern when scaling up services in the community. We are ensuring community workers are trained on confidentiality and potential issues related to this are monitored continuously and addressed through further training and supervision.
In terms of key lessons that we learned from this experience, the first is that there are a lot of unemployed and capable people in the communities that can scale up community service delivery by supporting case finding, providing adherence counselling, and refilling medications. We were also surprised to find out that many newly enrolled patients on MMD are adhering to treatment. This evidence can possibly result in policy changes at the World Health Organization, which currently recommends MMD for only stable patients – those who are virally suppressed. The fact that we are finding patients who are not considered stable adhering to treatment shows progress in this area.
*Banner image caption: Shutterstock.com
Posts on the blog represent the views of the authors and do not necessarily represent the views of Chemonics.