Innovations for Maternal and Newborn Health: Getting from “Great Ideas” to “Global Lifesavers”
October 12, 2017 | 4 Minute ReadPam Bolton and Emma Clark discuss the magic word that is helping save lives in global health.
Think we’ve made progress in maternal and newborn health (MNH) in the past 30 years? You’re right: Maternal mortality has dropped from 550,000 deaths due to pregnancy-related causes a year to 303,000, and newborn mortality from 4.4 million to 2.7 million newborns each year. But if you think that still sounds like a lot of deaths, you’re also right: 830 women and 7,000 newborns are still dying every day — deaths that are nearly all preventable (WHO, 2016).
The global health community has been scrambling for ways to save more lives, faster, and to help those who survive also thrive. Often, that magic word “innovation” is floated as the answer. But great ideas can only become global lifesavers if we as an international community throw our expertise and support behind the people with the great new ideas.
From global neglect to global goals
MNH innovation is taking place in a landscape that has evolved dramatically over the past 30 years. The Nairobi Safe Motherhood Conference in 1987 put maternal health on the agenda for the first time, issuing a call to action to cut maternal deaths in half by 2000. Though we didn’t achieve that target, the Safe Motherhood movement was instrumental in getting maternal health included in the Millennium Development Goals (MDGs), which aimed to decrease maternal mortality by 75 percent by 2015.
At first, progress was slow, but in 2010 the U.N. Secretary General launched the Every Woman Every Child movement and a new Global Strategy for Women and Children’s Health (an even more recent version is available here). Progress picked up. (Reanalysis of the data by WHO and others also helped.) By 2015, the 1990 maternal mortality had nearly been halved — a major improvement but vastly short of the target. The MDGs’ successors, the Sustainable Development Goals, set a new goal of decreasing maternal mortality to fewer than 70 maternal deaths per 100,000 live births by 2030. This requires an annual rate of reduction of at least 7.5 percent, or more than double the annual rate of progress made from 2000 to 2015. What will we have to do to achieve this? Well, innovate!
Let 1,000 flowers bloom: Incentivizing MNH innovation
To paraphrase the scientist and two-time Nobel laureate Dr. Linus Pauling, “To have a good innovation you must have many innovations.” The Bill & Melinda Gates Foundation kick-started a big push for MNH innovation when, in 2008, it sought “bold and inventive ways” to deliver MNH solutions to the poorest. The new attention and funding directed to MNH innovation created a groundswell of effort. It spurred NGOs to try new approaches, such as crowdsourcing ideas in African communities, and attracted new entrants to the field, including universities and innovators from low and middle income countries. The latter now account for as much as 50 percent of grant applicants.
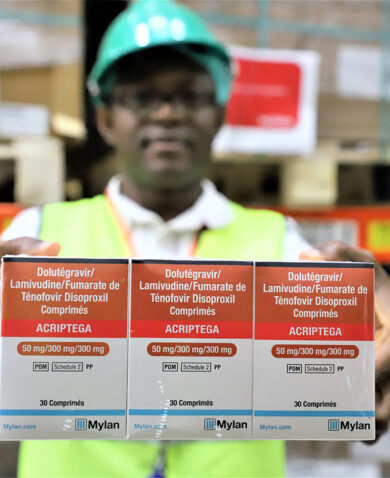
The Gates Foundation, Clinton Health Access Initiative, and others also tried out new ways to remove —or mitigate — some of the economic risks that come with introducing innovations in low-income settings. These novel approaches have incentivized more businesses to get involved, pursue cross-sectoral partnerships with NGOs and universities, and find novel ways to meet the health needs of moms and babies much further down the economic pyramid. As a case in point, Philips Healthcare is investing heavily in maternal/newborn innovation in Africa and has partnered with UNICEF and Concern Worldwide to support the Maker Hub for MNCH at the University of Nairobi Science & Technology Park.
Governments, too, have designed new efforts to incentivize and reward innovations that demonstrate potential to save lives. USAID, for example, participates in several flagship innovation initiatives. Likewise, both the Global Innovation Fund, a USAID spin-off, and the Grand Challengescontest series, sponsored by several government donors, have funded exciting and novel products and programs.
Attracting investors to an innovation “marketplace”
To be a global lifesaver means getting to large scale — reaching millions — and that’s still the tough part. It needs big money. In talking about the progression to scale, Grand Challenges Canada Executive Director Dr. Peter Singer draws the analogy of innovators climbing a ladder with several missing rungs. They get stuck.
But there’s a growing effort to match promising innovations to prospective investors, in part by finding new ways — sometimes with state-of-the-art modeling techniques — to project (and compare) the future value of a new technology in lives saved. For example, the Augmented Infant Resuscitator (AIR), a device providing instant feedback to health workers helping newborns breathe, won a Saving Lives at Birth Transition-to-Scale grant in July based in part on its potential to save 1.8 million newborns a year. Grand Challenges and USAID’s Development Innovation Ventures (or DIV) similarly offer staged financing that ramps up exponentially as innovations progressively prove themselves.
The Every Woman Every Child Innovation Marketplace plays a vital matchmaker role, introducing innovators who demonstrate early success to governments, philanthropists, multinational corporations — even venture capitalists — that are ready to invest. At the Innovation Marketplace held during last month’s U.N. General Assembly, for example, AIR was pitched alongside a promising new low-cost device called InPress to treat postpartum hemorrhage, the number one cause of maternal death. These “brokered” introductions to funders add rungs to the ladder.
The unprecedented interest in innovation from both the public and private sectors combined with the desire to meet global targets means we’ve got incredible momentum to improve MNH and save more lives. We must take advantage of the momentum to keep the trend accelerating and hit those ambitious 2030 goals.